By Stefan Alius, Global Lead Poultry
Each year, national, regional and global human health organizations publish the occurrence of the main zoonoses. Salmonellosis, Campylobacteriosis and Colibacillosis are the 3 main foodborne illnesses worldwide, causing millions of people to suffer from intestinal problems, perhaps requiring hospitalization, and even resulting in death.
Part of the incidence of these zoonoses is attributed to poultry – mainly eggs or poultry meat (broilers or turkeys). Although, in general, Salmonella or Campylobacter contamination has no negative impact on poultry health, E. Coli contamination frequently affects the general health and performance of poultry. This already gives the poultry producer a first sign that he should be alert to the increased risk to the consumer, and this risk should be further communicated down the production chain. As poultry are rarely negatively affected by the non-host-specific serotypes of Salmonella or Campylobacter, the only way to assess risk is by frequently monitoring the presence of the bacteria in the poultry and further in the production process. Thanks to stringent regulations developed by the national authorities, great strides have been made in this over the last few decades. Yet, despite all of the efforts, these zoonoses persist.
Salmonella contributes to the environment, so it will always be present
As we focus on Salmonella and Salmonellosis in this article, we need to emphasize that Salmonella bacteria are present in the overall environment and that the non-host-specific serotypes are pathogenic to humans but not for poultry. Moreover, for plants, they are even beneficial, as they are part of the ecological process in breaking down complex organic material into smaller and simpler molecules. Even in poultry production, some serotypes can have a positive effect on production. This recycling of nutrients improves soil fertility and contributes to plant-soil interaction. This also explains why Salmonella can be found everywhere and not only in livestock.
Salmonella itself can survive under harsh and extreme conditions. They can grow in a temperature range of 5° to 46° Celsius, if the culture pH is 5.5 or more with a water activity (Aw) of at least 0.94. If the pH is less than 4.5, and the Aw is less than 0.94, growth becomes difficult. This is also why, in poultry, if Salmonella is present, you will find it more in the ceca (higher pH and higher Aw). Understanding its reservoirs and transmission routes is essential to developing a strategy to control Salmonella contamination in poultry and to reduce the risk of Salmonellosis. Poultry harboring the bacterium without any symptoms is the biggest risk to food safety. One animal that’s positive in a flock can have a significant impact on the spread of Salmonella within the flock, due to increased shedding in the feces during stressful circumstances such as overcrowding, catching, and transportation.
Salmonella cells can survive freezing, or even drying, without losing their ability to become pathogenic. Salmonella can survive even in an environment rich in salt. Like the increased risk of mycotoxins being present in cereals due to climate change, Salmonella can be present for the same reason. Higher temperatures and increased precipitation help Salmonella survive and multiply faster in nature. As Salmonella is part of the process maintaining ecological balance, the most common natural reservoirs from which it all starts are the water sources and the soil. Salmonella bacteria have the ability to create a biofilm to protect themselves against harsh circumstances or antibacterial products – but they also have other mechanisms to survive and compete with other microorganisms for the necessary nutrients or to move to better locations for survival, growth and multiplication (e.g., virulence factor and invasiveness). Figure 1 shows the direct and indirect Salmonella transmission routes between animals and humans, as well as the mechanisms to survive, grow and multiply in both human and animal bodies.
Reducing the risk of Salmonellosis entails interrupting these transmission routes, either by improving biosecurity processes ((personal) hygiene, cleaning, disinfection, bird- and rodent-free housing, no pets, etc.) or by reducing the shedding of Salmonella (by which the soil or water can become contaminated, creating a vicious circle of contamination, cross-contamination, and re-contamination).
How to reduce the risk of Salmonella contamination
This article does not present biosecurity measures that can be taken to reduce the risk of Salmonella entering the poultry production chain; instead, we briefly outline a strategy by which you can reduce the risk of Salmonella in poultry by focusing on the animal itself and by focusing on Salmonella behavior in the animal.
1. Determine the risk factors
To protect your brand and reduce the risk of recalling your poultry meat or eggs due to Salmonellosis, you need to practice a monitoring program to detect the presence of Salmonella inside the poultry house as well as in the broader environment outside the production unit, and you need to determine the risk of transmission to the poultry inside the poultry house. Conservative data show that, on average, over 4% of poultry meat and eggs worldwide still test positive for Salmonella, which indicates that ‘zero risk’ does not yet exist. So, the first step is to identify where in your operation the risk of the presence of Salmonella is highest.
2. Focus on reducing the risk factors in your production process
The second step is to focus on this specific risk to reduce the possible presence of Salmonella in all of the equipment, animals, handling activities, supplies, and so on.
The risk of the presence of Salmonella in the environment can be quite different between companies. If you are located in a humid tropical region, close to a lake, where wild animals come to pasture and drink, the risk of contaminated rodents and insects surrounding (and probably entering) your poultry house is greater than when you are located in a region in which the temperature is rarely above 10° Celsius with no nearby lake. Research has indicated that, in Thailand, between 49% to 75% of the flocks become Salmonella-positive due to rodents and insects.
Of course, the biggest risk of the presence of Salmonella is when your previous flock was contaminated with Salmonella and you start emptying the contaminated litter from your poultry house – especially when you store it for some time near the poultry house before it is carried away. This is a major cause of Salmonella spreading in the environment of your operation, very often without the possibility to control, clean and disinfect the outside environment. The risk of vectors becoming positive in this way is high, which again poses a big risk for the next flock once it enters the poultry house.
3. Salmonella: from source to target – how to reduce the transmission
The final step is to improve the resistance of poultry that are susceptible to Salmonella contamination. It is well known that the poultry’s age and general health have a significant impact on the risk of transmission of Salmonella. Broilers are more sensitive to Salmonella contamination during the first 10 days, because their natural immune system is not fully functioning. In general, in a healthy flock becoming Salmonella-positive, 5% to maximum 10% of the chickens will become positive. When poultry are sick or stressed – during thinning or transportation, for instance – much more Salmonella is excreted, which increases the risk of a higher percentage of your flock becoming Salmonella-positive at the time of slaughter. But even this does not mean that your meat or eggs become positive. By focusing on the animal itself and the behavior of Salmonella in the animal, steps can be taken to minimize the success of the transmission route.
The transmission route is ‘successful’ if, in a Salmonella-positive environment, poultry and poultry meat become Salmonella-positive. To prevent this, we can apply two main principles: first, by working on the bacteria once they have entered the gastro-intestinal tract; and secondly, by working on the animal itself to stimulate its self-defense system.
S-prove, a functional feed ingredient from Agrifirm, works on both principles.
| Butyric acid (0.03%) | S-prove (0.03%) | |
|---|---|---|
| Kill of (%) | 70,0 | 97,64 |
| Survive (%) | 30,0 | 2,36 |
| Invasion efficiency (%) | 4,35 | 1,69 |
| Virtual risk on Salmonella contamination (%) | 1,31 | 0,04 |
S-prove: Salmonella-proof thanks to its direct and indirect antibacterial effects
S-prove has strong antibacterial activity against Salmonella for both host-specific (S. Gallinarum, S. Pullorum) and non-host-specific serotypes (e.g., S. Enteritidis, S. Typhimurium, S. Java, S. Infantis, etc.). S-prove destroys the bacterial cell membrane so that the cell content starts to leak out, weakening the bacteria and eventually resulting in cell death. In addition, due to its composition, S-prove can easily enter the bacteria through these holes and release protons to acidify the cell content, quickly resulting in bacterial death. Furthermore, once the protons are released, the negatively charged molecules intercalate with the bacteria’s DNA so that it can no longer duplicate itself before bacterial death.
S-prove’s antibacterial activity, combined with limiting the duplication of the bacteria, has a positive impact on the reduction of the excretion of Salmonella via the feces, reducing the total bacterial load in the poultry house and, as a consequence, reducing the risk of cross-contamination. In addition to this antibacterial effect on Salmonella, S-prove also impacts the gene expression that is responsible for the virulence of the bacteria, which greatly reduces their ability to invade the blood stream and spread to organs other than the gastro-intestinal tract. Thus, it also prevents muscles and organs from becoming contaminated before harvest.
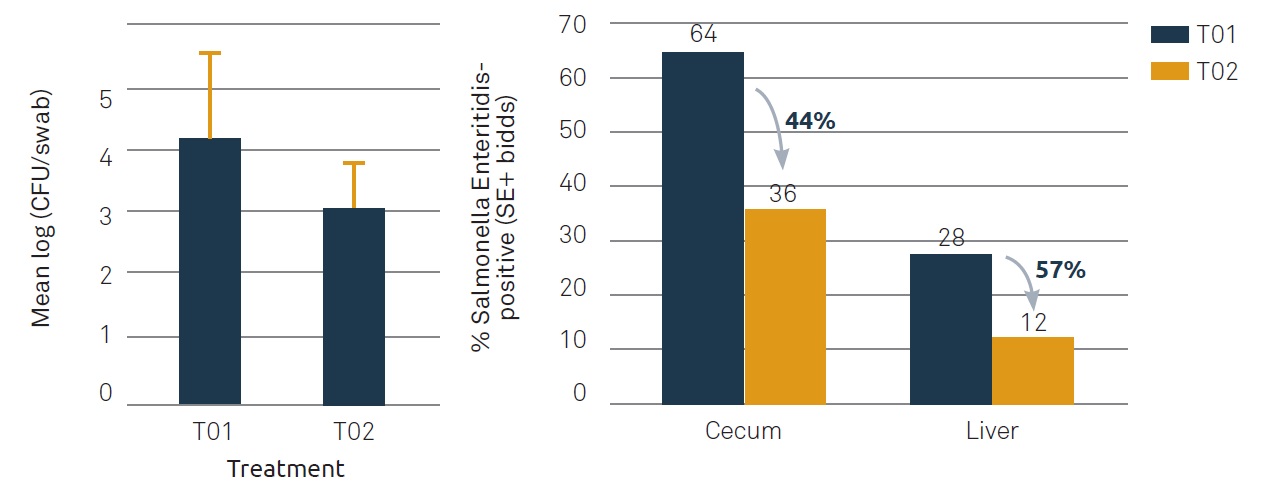
In vitro and ex-vivo studies have shown that, via this way, the transmission route can be blocked by 99.9% (Table 1). In vivo work (challenge trial, infected at day 7 with S. Enteritidis, 1.6* 10³ CFU/bird) shows that S-prove, at day 12, is capable of reducing the presence of Salmonella in the cloacal swabs (Mean Log CFU/g cloacal swab, p<0,053) of birds, reduces the number of birds with positive cecal content by 44%, and reduces the number of birds that became positive in the liver (indicating after invasion) by 57% compared to the control group (Figure 2).
This research confirms that poultry are capable of resisting Salmonella contamination – and also that S-prove can further reduce the Salmonella contamination of organs (either meat or eggs) from 57% down to 12%. Besides the effect on Salmonella itself, how can S-prove have this significant effect on reducing the transmission to the animal? This is mainly due to the cell-mediated and humoral immune response of the innate and adaptive immune systems. Goblet cells, responsible for the secretion of mucus, are part of the first-line defense, reducing the possibility for Salmonella to adhere to the epithelial cells. As S-prove increases the number of Goblet cells, it reduces the possibility of Salmonella to adhere to, and invade, the epithelial cells and move to the blood stream and other organs.
Poultry possess the capacity to secrete avian β-defensin 9, which is an anti-microbial peptide that kills Salmonella as part of the innate as well as the adaptive immune systems. Secretion is done primarily by the spleen, and S-prove stimulates the secretion of avian β-defensin 9 in the spleen significantly – hence, increasing the animal’s antibacterial activity. Research conducted at the University of Veterinary Medicine in Vienna has shown that S-prove increases the number of T-cells. Both CD4+ and CD8+ cell numbers were elevated; but the activated cytotoxic CD8+ cells (CD8CD25), in particular, were significantly increased, indicating that the cellular adaptive immune system has a higher capacity to kill the bacterially contaminated cells. In addition to this specific killing activity of the active CD8+ cells, CD4+ cells also initiate the secretion of several pro-inflammatory cytokines, as required. This means faster and more efficient response against antigens. Although T-cells are part of the adaptive immune system, they are often considered to be the bridge between the innate and the adaptive immune systems. Earlier research by Wang et al (2023) has proven that poultry with a reduced H/L-ratio (heterophil/lymphocyte ratio or ‘innate/adaptive’) are more resilient to Salmonella infections.
Conclusion
Successfully preventing Salmonella contamination can only occur when proper risk determination has taken place to identify the main sources of contamination or re-contamination – not only in the poultry houses but also in the broader environment. Focusing on the activities or animals that pose a risk is not sufficient to reduce the incidence of Salmonella-positive birds in your operation. Working on the transmission route by increasing the natural resistance of poultry to Salmonella contamination and by enhancing the antibacterial activity against Salmonella in the animal is crucial in safeguarding your product, your brand name, and your profitability.